A senior at Cornell College in Mount Vernon, Iowa, engineering major Nicholas Bieno spent the past summer collaborating with professor Brian Johns on a virtual reality project.
The project is a surgical simulator that combines a virtual setting with tangible tools and will hopefully be used to train med students, giving them plenty of practice before performing on a real person.
August Pritchett: How did you start the collaboration?
Nicholas Bieno: I applied for the position along with several other people and professor Johns chose me out of all the applicants to work for him.
AP: What made you want to do this collaboration?
NB: I want to work with orthopedics and prosthetics, and this isn’t it, but it’s still close to what I want to do and it’s a good way to get your feet wet.
AP: Why did you want to work with prosthetics and orthopedics?
NB: Ever since I was young, I have played sports. I’ve been in and around athletics and one thing that happens often are injuries, and I didn’t like trying to treat them. It’s not really what I wanted to do, but I did like the math and sciences behind engineering.
I wanted to combine my passion for sports with something that could help other people get better or not get hurt as much. A lot of the work I’d probably be doing is for people who can’t really do things on their own, whether it’s from birth defects or car accidents. Just to help them live a normal life — I think that’s something everyone should be able to do.
AP: What was it like working on this project, and how did you come up with the idea to do a virtual reality surgical program?
NB: Dr. Johns did his PhD dissertation on a surgical simulator that was, at the time, kind of a cross between a computer-aided augmented reality, but it was before what virtual reality is today. Not to say virtual reality didn’t exist, but it wasn’t as prevalent and readily accessible, so a lot of what he did was simulating x-rays on a computer screen and having surgical residents trying to drill into a bone.
So, his PhD was more on the technical side of the things of how to get bones to accurately match up in real life. Primarily what I worked on this summer was updating his work to 2017 standards, working with brand-new technologies. The idea came from his PhD dissertation and we updated it.
AP: Why did you sign up for this project?
NB: Well, there are a couple of reasons. Number one was that it interested me. What I like to do is design things; I like to work with stuff that hasn’t been done before.
So, while this project isn’t 100 percent new, it was taking something that we had and pushing the boundaries of what we could do with it. And on top of that, it also dealt with topics that were close to what I wanted to do in the future with orthopedics and prosthetics. This has to do more with implants than either of those two, but it’s still in the same field of how we work with the thematics [sic] of the body to make things work together.
AP: What did you get out of working on this project?
NB: One of the really nice things about this project was that it didn’t just work with engineering. It had the medical side, obviously. There was also an art component I didn’t expect such as 3-D modeling, animation and putting things together. There’s a whole bunch of computer coding that I had to learn, and it was just a good way to get myself acclimated with different things I normally wouldn’t know how to do.
AP: Can you explain, in detail, what this simulator actually consists of?
NB: I think the easiest way to start is explaining what we’re trying to simulate. Oftentimes elderly and people of significant age have what’s called osteoporosis, which is the degradation of bone, and this leads to a point in the body—like the hips or the back—where large loads of weight are put; they’ll oftentimes have bone fractures and failures.
One of the more common ones is called an intertrochanteric fracture. It’s interior, like in-between tropanteric, which is a medical term for tropanter in the fracture. This fracture occurs when the little net between the femur (which is the part that makes your upper thigh) and the head (where it attaches to the hip) breaks away from the main shaft. That means you can’t walk on it because it’s a load-bearing area of the body, and in order to fix that, you have to have surgery performed.
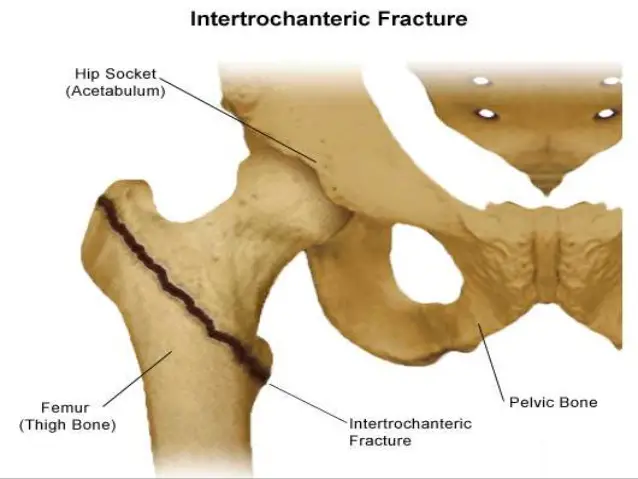
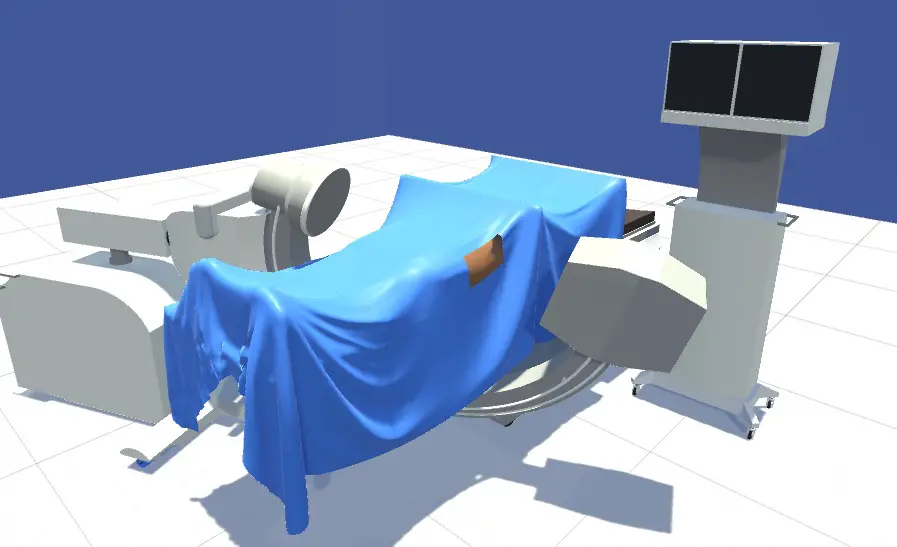
We’re trying to simulate the surgery you would perform to repair that fracture. What they essentially do is they take a bolt (it’s a fancy medical bolt, but it’s still essentially a leg bolt) and they put it into your femoral head—which is the ball that sits inside of the hip. Then they put in another piece called a sliding hip plate, which is essentially like putting in a nut and a bolt onto the femoral shaft and rationing the two together. It’s a little bit more complicated than that, but that’s kind of the simplified version of what this surgery actually does. And the difficulty of it is if you don’t put that bolt into the proper place in the hip, it’ll do what is called “cut-out,” and it means that it literally falls out. Yeah, it’s not good.
On top of that, because it’s all being done inside the bone, and you can’t see where you are, you have to take x-rays. Oftentimes, you take many of them, so both the patient and the surgeon have to shoot x-rays into their bodies in order to do this surgery, which is problematic if you’re trying to practice; doing it over and over with real x-rays is bad.
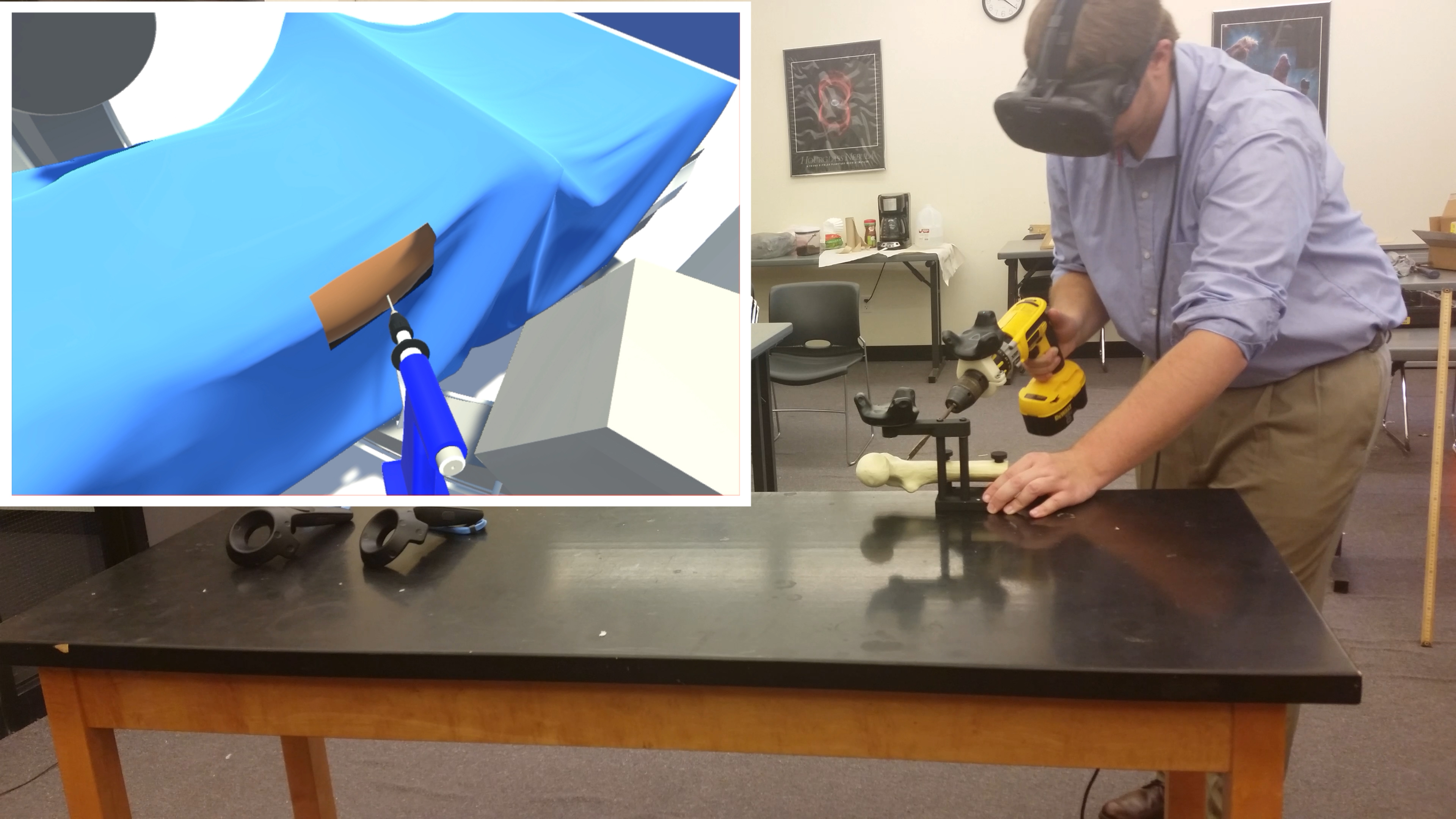
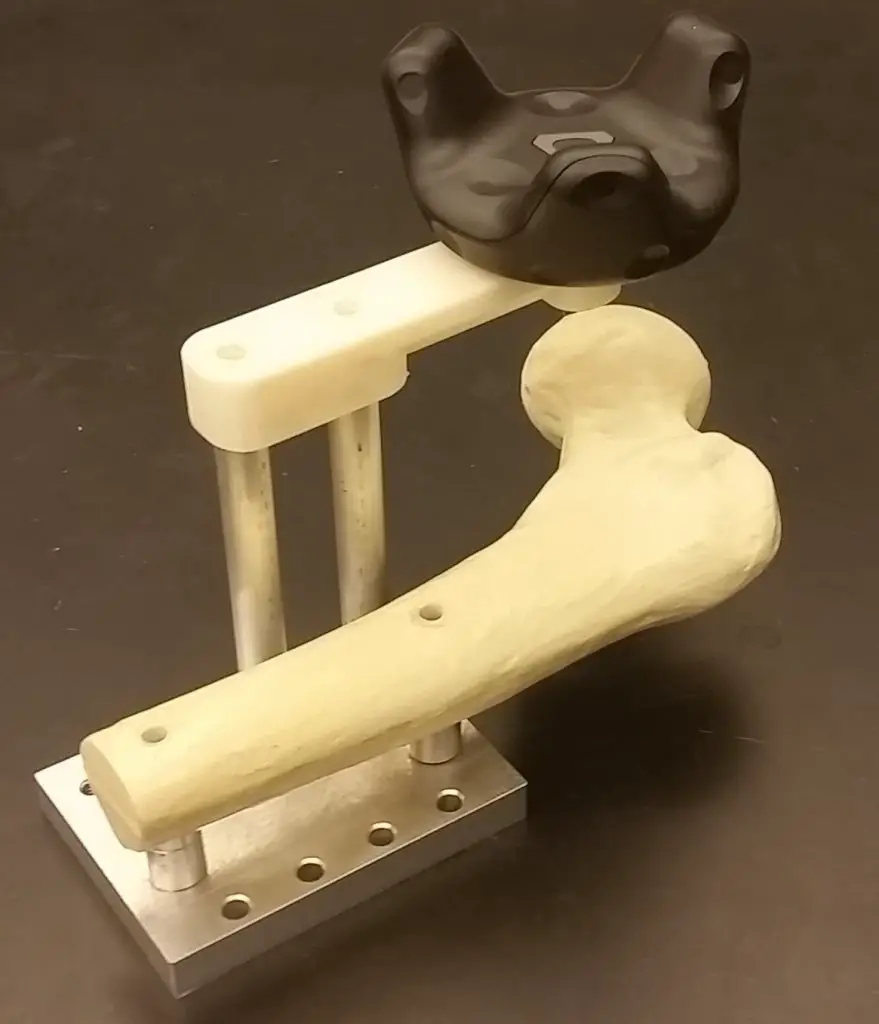
So, what we’re trying to do is take out both the x-rays and the real patient by essentially making a virtual world using computer graphics and computer programming. Then we are taking a synthetic bone that you can touch and feel as you’re drilling into it, so what you see is the operating room, the patient and the x-rays display; in reality you have a real drill in your hand and are actually drilling into a synthetic bone. So, you get both the feeling of being in an operating room and also the sensation of drilling into the bone.
AP: So, is it kind of like a virtual surgery game online?
NB: It’s sort of like a serious version of those, yes. It’s not intended for entertainment. I wouldn’t say that doing this simulator is entertaining (I’m not a surgeon, I don’t find drilling into things incredibly enjoyable), but to surgeons I’m sure it’s a little more enjoyable. It’s not a simulator intended for fun, it’s intended for education.
AP: What do you hope would be the outcome of all this?
NB: This is off the top of my head, but it is projected that in 24 years, there will be about fifty thousand hip fractures. As Americans become more obese, it will become a major problem when our generation or the generation before us get older because we will be so much heavier than we have been in the past. The hips will be failing at a higher rate.
By getting surgeons trained now who are able to perform this, we should be able to have enough expertise so when we eventually have this problem, we can properly deal with it. The hope is that this eventually becomes something that can help people not today, but in the future.
There’s a lot of stuff that has to be done with getting the simulator accredited and passed by all the bureaus and the government stuff that allows us to actually use it for educational purposes, so it’s not ready right this second. But, it’s hopeful that this could be used to teach surgeons to potentially help people in the future with the intent that the first time you perform the surgery, it’s on something other than on a real person.